Introduction
The Fluid Management module challenges students to broaden their differential diagnoses when approaching a patient who has abdominal pain. This can be applied to inpatient and primary care settings.
Content Contributors:
Author: Dr Richard Arnold
UPDATE AUTHORS: Dr Nicholas Hewett
ACCESSORY CONTENT: Dr Nicholas Hewett
EDITOR: Dr Amelia Welch
CONTENT APPROVAL: Dr Amanda Dawson
Version History
Version 1: 16 June 2016
Version 2: 1 July 2016
Version 3: 11 August 2016
Version 4: 17 September 2016
Version 5: 6 October 2016
Version 6: 23 October 2019
This module forms part of the Core Curriculum.
It requires 30 minutes preparation.
It can be taught in 1 hour
Preparation materials
Fluid order forms
Fluid balance charts
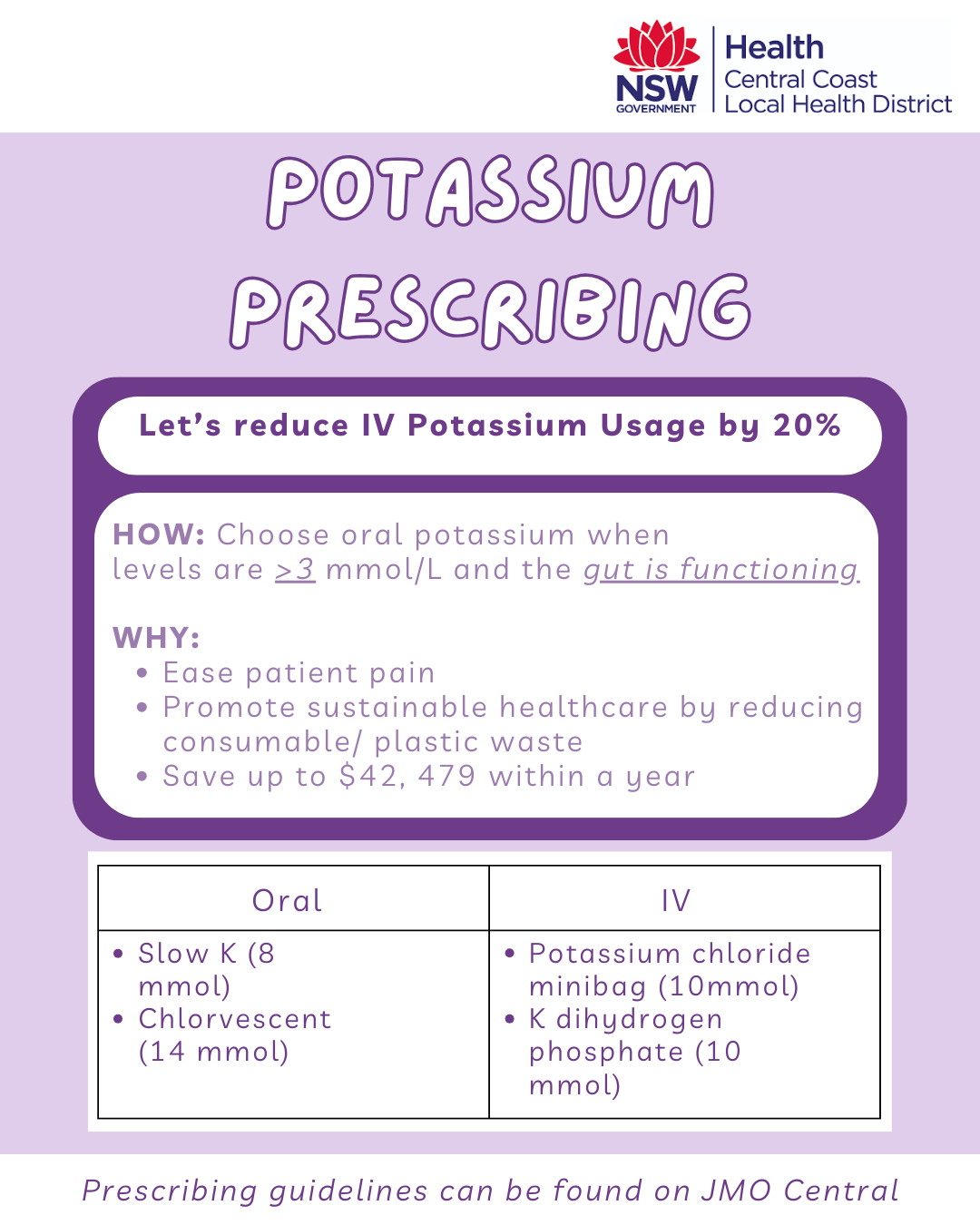
Physical samples of fluid and electrolyte products for students to handle (i.e Saline bags, Slow K tablets, lines, etc)
Teaching approach
As with all modules, familiarise yourself with the NPMT principles.
Fluid management is one of the most common activities of a junior doctor, yet it is one of the most challenging topics to teach effectively. We’ve found that a step-by-step approach, with a focus on clinical scenarios (rather than minute) is the most effective way to approach its.
This module aims to teach students to:
Understand the role of fluids and the body:
Fluid inputs and outputs
The fluid balance chart.
Understand how to conduct a fluid assessment.
Understand the fluid requirements a particular patient.
Familiarise themselves with key replacement products.
Introduced key electrolytes:
Understand common derangements and their presentation
Understand in general terms methods of electrolyte replacement.
Chart fluids with scenarios.
Tips & Tricks
Here are some tips how to run the session effectively:
Be as interactive as possible
Provide completed copies of fluid balance charts for each student too look over and review
Use clinical examples to illustrate the principles and components of a fluid balance exam
Make sure to allocate time for charting exercises and discussion of clinical senarios
Here are common pitfalls to avoid:
Getting lost in the details of the numbers and formulae
Focusing on the symptoms and signs of uncommon electrolyte disturbances
Going into the details of less commonly used colloids and crystalloids
From our feedback, the more interactive and ‘put on the spot’ you make the session, the more valuable it will be. Having students think on the spot and share their ideas in a non-threatening environment is key to making the session light-hearted and collaborative so that they can apply what they have learnt at medical school to a clinical patient.
Download Resources:
Other Resources
No prescribed resources. Instead, look at the files/images/documents which helped you learn fluid management. Adapt and use what worked well for you.
NICE Guidelines: Algorithms for IV fluid therapy